The science of mRNA vaccines: what are they and how do they prevent COVID-19
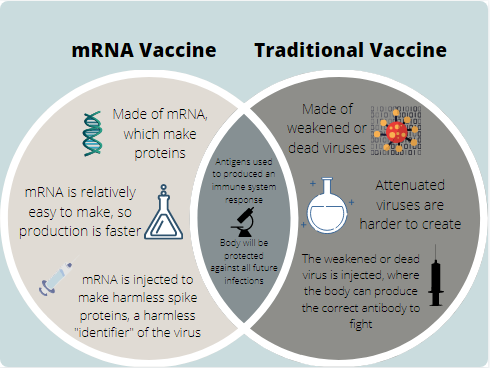
The image shows an image explaining the key similarities and differences between the traditional attenuated vaccines and the new mRNA vaccines.
January 18, 2021
Knowing that the FDA approved the Pfizer vaccine last month, people may wonder what the science behind these vaccines is, especially as the new Pfizer and Moderna vaccines are the first of their kind.
Despite having an almost 30- year-old history of scientific discoveries behind them, the Pfizer and Moderna mRNA vaccines remain confusing to many, but they’re actually not that complicated.
First of all, a mRNA vaccine is not the same as live vaccines, which are weakened or dead versions of the virus/bacteria they’re targeting. Live vaccines create immunity by stimulating the body’s immune system to produce antibodies will be produced, although with time. After the vaccination, the antibodies will be reused against the same specific antigen of a virus.
All other types of vaccines are live attenuated vaccines.
These can produce a so-called “herd immunity”, where a majority of the population become immune to a disease, decreasing the danger it poses to the group.
The Pfizer and Moderna vaccines are both known as mRNA vaccines. A mRNA vaccine provides instructions for the human body to produce what is known as a “spike protein”, more specifically known as a spike glycoprotein.
These glycoproteins are a part of a virus’s viral envelope and create the spikes on it’s outside. One subunit of the spike protein will bind to a host cell receptor, while the second subunit is responsible for the fusion of the viral envelope to the cell membrane.
These spike proteins are perfect targets for vaccines to target, as without them, the virus will not be able to penetrate the cell membrane.
The mRNA vaccine contains mRNA instructions to make the harmless spike proteins into a coating that will prevent enzymes from breaking down the foreign mRNA. The mRNA will then enter the dendritic cells, or macrophages. These cells will process the message encoded in the mRNA and begin making the spike protein from the cell’s own ribosomes.
From there, the antigen will cause an immediate reaction, signaling the immune system of the body to begin producing antibodies that fight against the SARS-CoV-2, or the COVID-19 virus. This means that the human immune system will essentially know how to protect against the virus in future encounters.
DNA will not be affected as the mRNA does not travel into the nucleus. Yet, more unknowns remain, such as whether COVID-19 can spread asymptomatically, even with the vaccination, or how the mutated versions will interact with the current developed vaccines.